Comprehensive Diabetes Care for DMH Clients (CDC)
Why is it important?
Department
of Mental Health (DMH) data demonstrates that while DMH Members receive
primary care at rates similar to other MassHealth populations, they
experience worse health outcomes and unhealthy behaviors. The
goal of the DMH measure is to: address DMH client access to primary
care clinicians (PCCs); develop a new model of engagement that
supports the Member to make personal choices about adopting health
strategies; and to methodically and effectively adhere to medical
recommendations for treatment and health related activities such as
diet and exercise, appointments, screenings, and lab tests.
How is it measured?
The percentage of MBHP DMH Members 18 to 75 years of age with diabetes (type 1 and type 2) who had each of the following:
1. HbA1c control (<8%)
2. Blood Pressure Control (<140/90)
3. Eye Exam (Retinal) Performed
4. Medical Attention for Nephropathy
How does MBHP perform?
MBHP's CY 2015 final diabetes rates fell at:
- HbA1c <8%: 39.89%
- Blood Pressure Control <140/90: 49.86%
- Eye exam: 34.29%
- Nephropathy: 88.66%
How does MBHP stack up to Medicaid providers nationally?
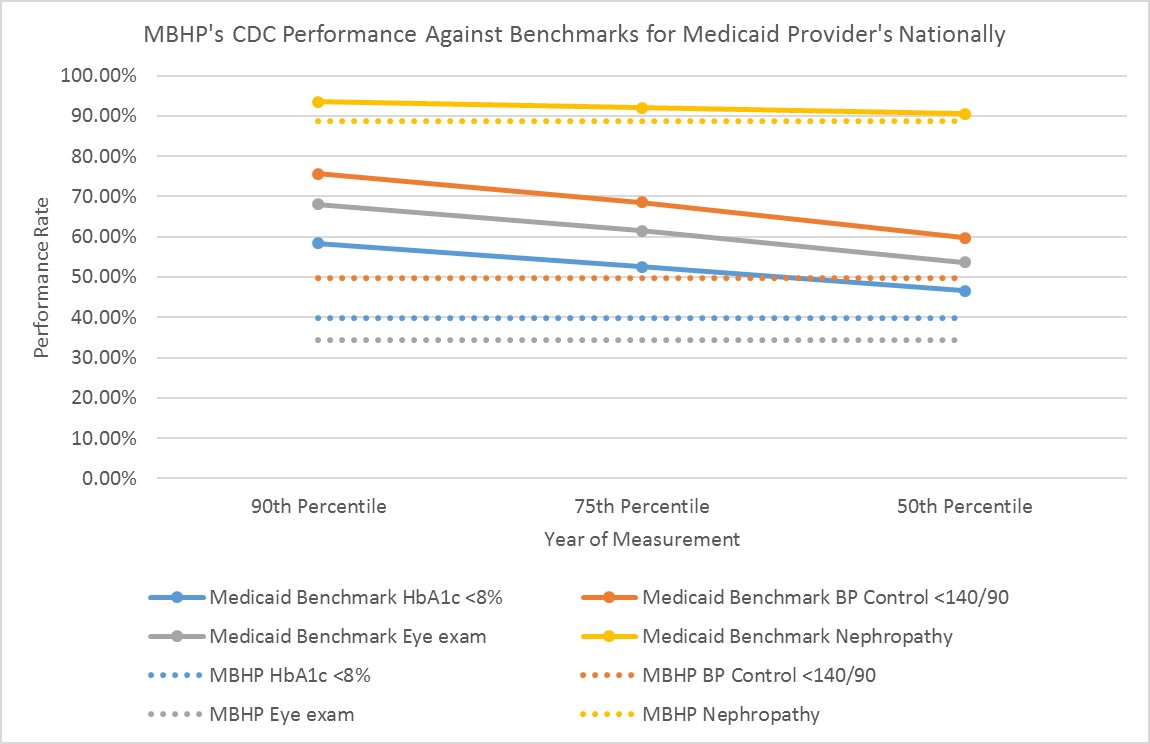
The figure below presents CDC benchmark rates across Medicaid plans nationally.
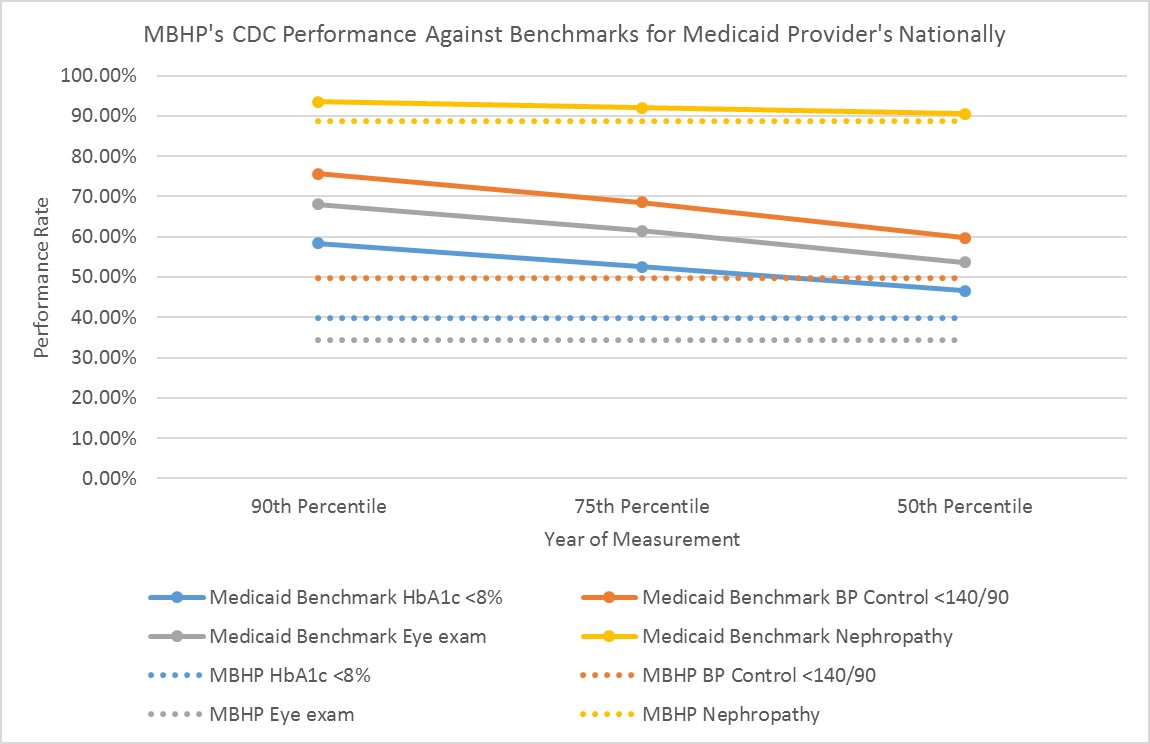
*Dotted lines represent MBHP Performance in 2015.
Performance goals
MBHP
has the goal of reaching the next highest benchmark of national
Medicaid providers Compressive Diabetes Care rates. Based on
current performance, MBHP has the following year-end goals for the
diabetes measure:
- HbA1c <8%: 50th Percentile= 46.64%
- Blood Pressure Control <140/90: 50th Percentile= 59.73%
- Eye Exam: 50th Percentile = 53.70%
- Nephropathy: 50th Percentile= 90.51%
Based on these benchmarks and MBHP's current performance, MBHP will need to improve HbA1c <8% by 16.92%, Blood Pressure Control <140/90 by 19.79%, Retinal Eye Exam by 56.61%, and Nephropathy by 2.09%.
What are our current improvement initiatives?
MBHP's
Quality Department is responsible for organizing improvement activities
and initiatives that support the CDC measure. Current efforts
include:
SSD: In
2015, MBHP will be responsible for reporting the HEDIS quality measure
Diabetes Screening Program for Members with Schizophrenia or Bipolar
Disorder who are Using Antipsychotic Medications (SSD). Routine
diabetes screening is important for people with either of these
diagnoses, particularly due to the added risk for diabetes associated
with antipsychotic medications. The SSD program will focus on
working with the BH provider network to improve rates of screening for
diabetes, with the intention of improving screening rates in the MBHP
network and strengthening lines of communication and care coordination
between the BH provider, PCC, and Member.
For more information on the SSD measure please see the SSD Provider Alert.
Collaboration with DMH to identify Members who are dually enrolled in DMH's CBFS program and MBHP's ICMP program:
MBHP aims to improve coordination between DMH case workers/CBFS staff
and MBHP's ICMP program in order to share information and better
coordinate care. MBHP will gather information on Members who use
both services in order to better coordinate between the services and
provide the highest quality care for our Members.
Outreach to Members through CSP Providers to support Members to schedule and get to appointments:
Many barriers such as transportation and access to necessary resources
can make it difficult for Members to get to diabetes-related care such
as the annual retinal eyes exam or nephropathy screening. CSP
providers can offer support to Members to overcome barriers in order to
increase rates of testing and treatment.
What can I do?
Follow best practices for treatment of diabetes:
- Test for HbA1c control (<8.0%), LDL-C
control (<100 mg/dL), and blood pressure control (<140/90 mm Hg) for Members with diabetes or those at
increased risk for developing diabetes as a result of taking an antipsychotic medication. If a
Member does not meet the requirement for control on these measures, coach him/her about a plan for diabetes control.
- Work
with Members to schedule a convenient time and location for the retinal
eye exam and nephropathy during your visit with the Member.
- Follow up with the Member's CSP or CBFS
provider to support the Member in getting a follow-up appointment.
Contact the Quality Department to access your DMH rate.